Pregnancy is a transformative journey filled with joy and anticipation, but for women with gestational diabetes, managing blood sugar levels becomes paramount for a healthy pregnancy. Fasting blood sugar control is particularly crucial during pregnancy to prevent complications and ensure the well-being of both mother and baby. In this comprehensive guide, we delve into effective strategies to control fasting blood sugar levels during pregnancy.
Table of Content
- Understanding Fasting Blood Sugar
- Why Fasting Blood Sugar Matters?
- Strategies for Healthy Fasting Blood Sugar
- Monitoring and Support: Working with Your Doctor
- Considerations for Specific Needs
- Gestational Diabetes: When Extra Support is Needed
Understanding Fasting Blood Sugar
Fasting blood sugar, or fasting plasma glucose (FPG), is a measure of the amount of glucose (sugar) in your blood after not eating for at least eight hours. During pregnancy, it’s important to understand fasting blood sugar levels because the placenta produces hormones that can make it harder for your body to use insulin.
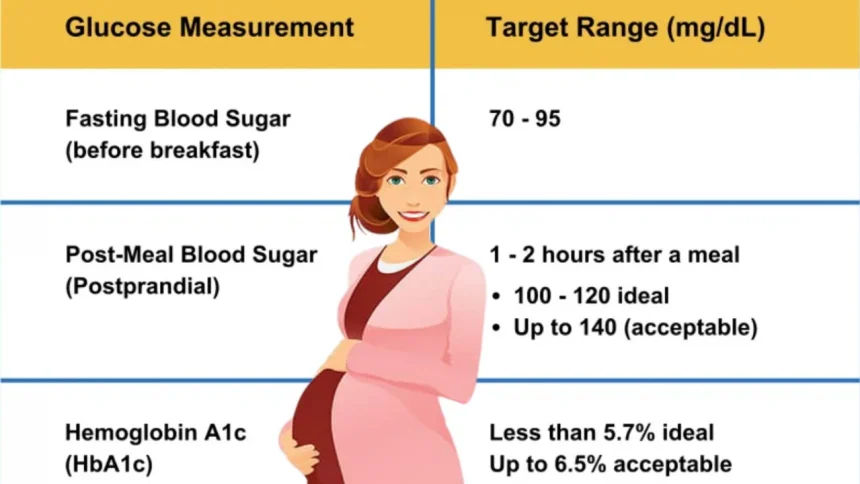
Here are some normal blood sugar levels for pregnant women:
- Fasting: 70–95 mg/dL
- Before a meal: 95 mg/dL or less
- 1 hour after a meal: 140 mg/dL or less
- 2 hours after a meal: 120 mg/dL or less
To control fasting blood sugar during pregnancy, you can:
- Eat three small meals and three to four healthy snacks every two to three hours
- Don’t skip meals or snacks
- Have a bedtime snack

Why Fasting Blood Sugar Matter?
Fasting blood sugar levels during pregnancy are important for several reasons:
Gestational Diabetes Risk:
Elevated fasting blood sugar can indicate gestational diabetes, which can lead to complications for both the mother and baby if not managed properly.
Fetal Development:
High blood sugar levels can affect fetal development, leading to potential issues like excessive growth (macrosomia) or developmental problems.
Maternal Health:
Proper blood sugar management helps reduce the risk of pregnancy-related complications, such as hypertension and preeclampsia.
Long-term Health:
Monitoring fasting blood sugar can help identify women at risk for developing type 2 diabetes later in life, allowing for early intervention.
Overall Well-Being:
Maintaining stable blood sugar levels contributes to overall health and energy levels during pregnancy, which is crucial for both the mother and baby.
Strategies for Healthy Fasting Blood Sugar
Now that we understand the significance of controlling fasting blood sugar, let’s explore some key strategies:
Embrace a Balanced Plate:
Food plays a pivotal role in managing blood sugar. Here are Dr. Shikha’s recommendations for a blood sugar-balancing diet during pregnancy:
Focus on whole grains:
Opt for whole grains like brown rice, quinoa, and whole-wheat bread over refined carbohydrates like white bread and pasta. These release sugar slowly, preventing spikes.
Add Fibers:
Include plenty of fruits and vegetables in your diet. Fiber helps regulate digestion and slows down sugar absorption.
Include Protein-Rich Foods:
Include lean protein sources like fish, chicken, beans, and lentils in your meals. Protein helps you feel satisfied and prevents blood sugar dips.
Healthy Fats:
Incorporate healthy fats like avocados, nuts, and olive oil into your diet. These keep you feeling full and support a healthy pregnancy.
Limit Sugary Treats:
Avoid sugary drinks, processed foods, and sweets. These can cause blood sugar spikes.
Monitoring and Support
Absolutely, working closely with your doctor during pregnancy is crucial for both your health and your baby’s well-being. Here are some key aspects of monitoring and support to consider:
Regular Check-ups
Schedule Appointments:
Regular prenatal visits allow your doctor to monitor your health and your baby’s development. Usually, visits are more frequent in the third trimester.
Ultrasounds and Tests:
Your doctor may recommend ultrasounds and various tests to assess growth, screen for abnormalities, and check your overall health.
Nutrition and Lifestyle
Dietary Guidance:
Discuss your nutritional needs. A balanced diet is vital for your baby’s development. Your doctor can provide guidance on what to eat and any necessary supplements, like folic acid or iron.
Exercise Recommendations:
Stay active, but check with your doctor about safe exercise routines during pregnancy.
Managing Symptoms
Addressing Discomfort:
Talk about any pregnancy symptoms, like nausea, fatigue, or swelling. Your doctor can suggest ways to manage these issues effectively.
Mental Health Support:
Pregnancy can be emotionally challenging. Don’t hesitate to discuss feelings of anxiety or depression; your doctor can provide resources or referrals.
Monitoring Conditions
Preexisting Conditions:
If you have conditions like diabetes or hypertension, your doctor will monitor them closely to ensure a healthy pregnancy.
Gestational Conditions:
Be aware of potential pregnancy-related conditions, like gestational diabetes or preeclampsia, and communicate any symptoms you experience.
Birth Planning
Discuss Birth Plans:
Talk about your preferences for labor and delivery. Understanding your options can help you feel more prepared.
Emergency Protocols:
Be clear about signs that require immediate medical attention.
Open Communication
Ask Questions:
Don’t hesitate to ask your doctor about anything—no question is too small.
Share Concerns:
If something doesn’t feel right, let your doctor know. Your intuition is important.
Support Systems
Involve Partners: Encourage your partner or support person to attend appointments with you. They can help remember information and provide emotional support.
Seek Additional Support: Consider joining a prenatal class or support group to connect with other expecting parents.

Considerations for Specific Needs
Your body has increased nutritional needs during pregnancy — you’re feeding a whole new person! Although the old adage of “eating for two” isn’t entirely correct, you do require more micronutrients and macronutrients to support you and your baby.
Micronutrients are dietary components, such as vitamins and minerals, that are only required in relatively small amounts.
Macronutrients are nutrients that provide calories, or energy. We’re talking carbohydrates, proteins, and fats. You’ll need to eat more of each type of nutrient during pregnancy.
Here are some general guidelines on a few important nutrients that will need to be adjusted based on your needs:
| Nutrient | Daily requirements for pregnant women |
|---|---|
| calcium | 1200 milligrams (mg) |
| folate | 600–800 micrograms (mcg) |
| iron | 27 mg |
| protein | 70–100 grams (g) per day, increasing each trimester |
Most pregnant people can meet these increased nutritional needs by choosing a diet that includes a variety of healthy foods such as:
- protein
- complex carbohydrates
- healthy types of fat like omega-3s
- vitamins and minerals
Gestational Diabetes
Gestational diabetes is diabetes diagnosed for the first time during pregnancy (gestation). Like other types of diabetes, gestational diabetes affects how your cells use sugar (glucose). Gestational diabetes causes high blood sugar that can affect your pregnancy and your baby’s health.
While any pregnancy complication is concerning, there’s good news. During pregnancy you can help control gestational diabetes by eating healthy foods, exercising and, if necessary, taking medication. Controlling blood sugar can keep you and your baby healthy and prevent a difficult delivery.
If you have gestational diabetes during pregnancy, generally your blood sugar returns to its usual level soon after delivery. But if you’ve had gestational diabetes, you have a higher risk of getting type 2 diabetes. You’ll need to be tested for changes in blood sugar more often.